Lack of accessibility to trans healthcare disproportionately impacts the community in Canada
- Nitika Mishra
- Aug 10, 2022
- 10 min read
Updated: Aug 15, 2022

Image Credits: Unsplash/Karollyne Hubert
A report by Statistics Canada shows that trans people are more vulnerable in the province in terms of their finances and health as compared to their cis-gendered peers.
Transgender Canadians were also more likely to have seriously contemplated suicide in their lifetimes. They were also more likely than cisgender Canadians to have been diagnosed with a mood or anxiety disorder, says the report.

Image: Dr. Tehmina Ahmad, She/Her / Transhealthto
Dr. Tehmina Ahmad, an Endocrinology and Metabolism Fellow at the University of Toronto, and incoming Women’s College Hospital Fellow with a specialty interest in transgender healthcare, said barriers faced by trans people while accessing healthcare needs to be removed
“Trans people today deserve appropriate healthcare, that means we have to start viewing gender expression and identity as protected by human rights law,” she said. “They are technically protected, but social norms of transphobia still mean that trans patients may encounter misgendering, inappropriate questions about their gender or sexuality, hyper-focus on sexual risk factors for health at the expense of other health issues.”
Ahmad said there are usually three ways barriers could be removed legally, socially and structurally.
Trans patients need to know their rights and lawyers may need to make clear to doctors, administrative staff, and others the importance and relevance of ‘reframing’ and reaffirming gender.
A sociocultural approach involves the long-term goal of getting cis people to think critically about gender, she said.
Ahmad said structural change is needed through governance to bring forward universal pharmacare and address the under-housing crisis, unemployment, and poverty that often disproportionately impact trans and gender diverse people, as these are socioeconomic drivers of poorer health status.
“Just as feminist movements of the 70s and 80s had implications not only for women in the workforce, but spearheaded changing norms of masculinity, so too acceptance of trans people, in general, should broaden societal views on what gender is, or can be, for everyone,” she said.
Ahmad was among the group that created Transhealthto, a website for healthcare providers to learn more about LGBTQ+ community with an emphasis on providing transgender care.
“Organizational change needs to occur to fully integrate and normalize trans patients, their health, and their overall experiences as part of regular medical care,” she said. "This involves years of unlearning and re-learning to continue to know, acknowledge, and validate trans and gender diverse individuals for who they are.”
Wisdom2Action , a non-partisan social enterprise, launched TransHealthOntario , a campaign to support the passage of Bill 17, the Gender Affirming Health Care Advisory Committee Act , a private member’s bill tabled by Toronto Centre MPP Suze Morrison. It reached the Standing Committee on Social Policy before the recent election.
TransHealthOntario noted trans people are among the most impoverished demographics in Ontario and often need to pay out of pocket “for procedures that are recognized as medically necessary.”
There are other barriers to trans healthcare in Ontario including long wait times, lack of knowledge about trans-affirming healthcare, usage of incorrect pronouns and lack of trans-competent doctors and physicians. Social Barriers make the lives of the trans persons extremely difficult, the campaign stated.
Trans Health Ontario said despite being recognized as medically necessary, many gender-affirming procedures including chest contouring and masculinization, tracheal shaves, voice modification surgery, permanent hair removal, and more, are not covered by OHIP.
Those medically necessary transition-related healthcare costs can be as high as, or even exceed, $45,000 and most of the time, the people in need of the mentioned surgeries, pay from their own pockets.

Image Credits: transhealthontario.org
An open letter from 48 LGBTQ+ and allied organizations was published calling for all Ontario political parties and leaders to support gender-affirming healthcare dubbed Bill 17
“Bill 17 is an important first step to improving coverage of medically necessary health services for trans, non-binary, intersex and gender diverse people in Ontario, and addressing the many barriers trans, non-binary, intersex and gender diverse people face in accessing both general and trans-specific healthcare.” the letter stated.
An extensive report published by Trans Pulse in 2015 detailed the level of discrimination, violence and exclusion faced by trans people in Ontario.
It stated that 96 per cent have heard that trans people were not normal whereas 73 per cent had been made fun of for being trans. Around 78 per cent reported their family had been hurt or embarrassed. These daily indignities can take their toll with 77 per cent worried about growing old as a trans person and 67 per cent fearing they would die young.
The report says one in 10 trans people who had accessed an emergency room presenting their gender identity had been refused care or had care terminated prematurely, because they were trans.
One-quarter reported being belittled or ridiculed by an emergency care provider for being trans. Among those with a family physician, about 40 per cent had experienced discriminatory behaviour from a family doctor at least once- refusal of care, refusal of examining certain body parts, use of demeaning language, lack of respect for gender identity and pronouns and making transphobic jokes.

Image Credits: Trans PULSE
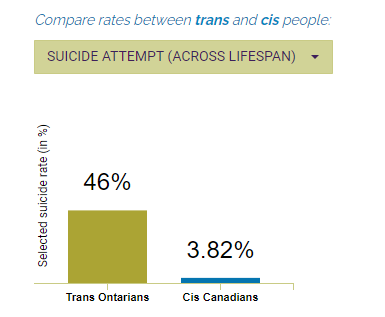
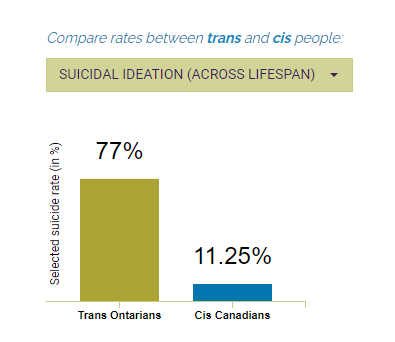
Rainbow Health Ontario explains the urgency of trans healthcare accessibility with its TransHealthGuide. It also states suicidal ideation and suicide attempt rates are alarmingly high among trans people. Providing support for medical transition can improve and impact their well-being.
-Credit: RainbowHealthOntario.org
Access to safe and medical transition is important because it directly impacts the well-being of trans people. Many trans people seek medical help so they can bring their physical appearance in line with their gender identity. This can include hormone therapy and/or surgery.
Researchers have revealed that safe and affordable completion of medical transition can substantially impact well-being and lower the risk of contemplating suicide. Below are two charts showing the suicidal ideation and attempt by trans people across all lifespans during various stages of their surgeries.
-Credit: RainbowHealthOntario.org
Transgender people in Ontario depend on family doctors for both general and transition-related care. However, a lot of the physicians have little to no training on trans healthcare and trans-specific guidelines. This coupled with a lack of affordability, forces them to avoid healthcare specific to their needs and requirements.

Jill Andrews, MPP, Toronto–St. Paul's / jillandrewmpp.ca
Jill Andrew, for Toronto-St Paul’s and the Ontario NDP Culture Critic and was the Women's Issues Critic for the Official Opposition, says more needs to be done to protect the lives and rights of the trans community of Ontario.
“Trans folks need to know that the surgeries they need, the medication they need are covered in Ontario because what happens when they are not is people aren’t able to live their fullest lives.” she said.
Andrew said more needs to be done although the Ontario NDP was able to achieve banning conversion therapy and was able to entrench transgender and gender-diverse people’s rights in the Ontario Human Rights Code 2012.
”We need to make all gender-affirming, transition drugs and therapy accessible and fully covered by OHIP.” she said.
Fellow New Democrat Morrison would require the Ministry of Health to form an advisory committee to review the state of trans healthcare in Ontario and make suggestions to the heath minister for improving access and coverage to gender-affirming healthcare in Ontario.
The committee would submit reports with comprehensive analysis and recommendations after consultation with trans, two-spirited, non-binary and gender-diverse communities’ , as well as relevant service providers, NGOs and stakeholders.
The health minister would be then required to inform the Queen’s Park of the recommendations to be implemented within 90 days of receiving a report.
Journals released by Trans PULSE in 2019, revealed there are significant disparities while accessing family physicians among transgender people in Ontario.
It was estimated that around 17.2 per cent of trans Ontarians did not have a regular family physician.
The report also revealed transfeminine persons - trans women and non-binary people assigned male sex at birth- who were Indigenous or POC were also less likely than other transfeminine persons to have a family physician.
Additionally, trans people who were homeless or had unstable housing were also less likely to have a family doctor than those who were adequately housed.
Another journal published by Trans PULSE in 2016 outlined various factors that impact transgender patients’ discomfort while dealing with their family doctors.
The survey reported that among 83.1 per cent of trans Ontarians who had a family doctor, almost half of them reported feelings of discomfort while discussing trans health issues while 37.2 per cent of transmasculine and 38.1 per cent of transfeminine people reported at least one negative experience while dealing with their family physicians.
Barriers to trans health care remain a challenge for trans people while accessing general or transition-specific health care needs. These barriers include lack of healthcare coverage at the provincial level, transphobia, lack of trans health trained physicians, discrimination, affordability , denial of care and lack of respect for gender identity and pronouns, the journal said.
Below the image shows the various kinds of barriers the trans community faces while trying to access healthcare.

Credits: RainbowHealthOntario.org
The Ontario HIV Treatment Network (OHTN) states that poor health outcomes are disproportionately experienced by transgender individuals and that coupled with socio-economic hurdles can increase the likelihood of poor health outcomes.
The report also explains combined layers of the stigma associated with transgender identity led to unique challenges individuals face while accessing quality and affordable healthcare. Those barriers can intersect or can act individually, depending on the person’s social, economic, and mental health situation.
Specific programs, therapies and services are necessary to address the existing disparities between transgender individuals and cisgender individuals while accessing healthcare.
Trans people are also at greater risk HIV and for poorer physical as well as mental health outcomes, the OHTN report states.
The U.S. National Transgender Discrimination Survey Report on Health and Health Care (NTDS) reported that transgender individuals in the United States experience over four times the national average of HIV infection, and are over 25 times more likely to have attempted suicide.
According to the NTDS, 19 per cent of transgender individuals reported that they had been homeless at some point in their lives while in Canada, the Trans PULSE survey reported 34 per cent of respondents were living in poverty, compared to 13.5 per cent of all Canadians. These disparities further contribute to the barriers the trans community faces in the healthcare sector.
Understanding the causes that prevent them from accessing healthcare including societal, environmental, legal as well as economic barriers is important for improving the overall health and well-being of the community in a province like Ontario.
The OHTN report found that to understand the factors that influence access to health care among transgender individuals on a holistic level, it is important to consider intersectionality.
An individual who identifies as a trans person can face multiple stigmas including stigmas based on gender identity, race, age, sexual orientation, socio-economic status as well as religious beliefs. Accessing health care is particularly complex for transgender individuals, who often have multiple marginalized identities.
Apart from this, individual-level barriers also affect a person’s ability to access health care. Individual barriers can stem from their lack of trust in the system which prevents them from reaching out to healthcare services.
This was explained in one Ontario based which concluded that 21 per cent of transgender participants avoid emergency services when needed for their mistrust of the system.
Mental health can also act as an individual barrier that may prevent people from accessing healthcare benefits. The Trans PULSE project in Ontario reported that 43 per cent of transgender individuals have attempted suicide and more than half of them experience symptoms of clinical depression.
Andrew, the first Black and queer person to be elected to the Ontario Legislature, said discrimination is faced by trans folks in each sector.
“We know that in Ontario, we experience homophobia, transphobia and biphobia,” she said. “We experience levels of discrimination in housing, education, healthcare and workforce,” she said.
Andrew said it is important for trans people to have access to mental health resources.
“Sometimes folks need to see a therapist to get through the feelings they have but they cannot afford it,” she said. “And that is just not okay in a province like Ontario.”
Lack of policies, transgender-specific information in healthcare, gender-diverse training amongst doctors and nurses and the overall erasure of trans needs significantly impacts their access and overall representation in the healthcare sector.
A report based in Ontario revealed that two types of erasures exist: Information erasure and institutional erasure.
Ahmad said a doctor has a unique role in being among the first in line to support an individual’s health including trans patients.
“Rather than 'silo-ing' trans health among a few practitioners that are ‘specialized’ in the field, we need to broaden knowledge of trans health concerns, such that they become a normalized part of training and professional development among all primary care physicians, where gender-affirming steps such as candidacy for surgical assessments or hormone-access are part of everyday practice.” she said.
She said practitioners should know the existing guidelines or seek activities to inform themselves of the current guidelines.
One Canadian study reported transgender individuals to feel the exclusion of transgender identity within the social environments of academic institutions potentially fuels the discrimination they experience regularly with health care providers.
The OHTN report outlines many surgeries are not covered in all provinces and territories.
Among those where coverage is available, some specific surgeries may not be included.
But to access these services, patients must meet the criteria for “gender dysphoria” as defined by the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).
This includes the strong and persistent discomfort with current sex that causes clinically significant distress in social or occupational functioning
Ttrans people must also meet eligibility as well as readiness criteria as explained in a study by Tiffany K Roberts, which can be an emotional, stressful and complicated process. The study also explained many procedures may be considered not necessarily due to incompatibility with patients’ genders and thus remain not covered by public health care.
The studies found by the OHTN report made recommendations to overcome such barriers while accessing healthcare for the trans community. Those were:
Coverage of transition-related surgeries and procedures under the public healthcare system without the need for a DSM-5 diagnosis. Implementation of guidelines at the provincial level to protect the community from any form of discrimination which includes denial of medical care under the pretext of “Medically unnecessary”.
Inclusion of trans-competent health care training into academic curriculums in medical and nursing institutes as well as residency training and licensing examinations. All doctors and nurses should be educated and trained enough to be able to adhere to trans-specific needs and care.
Implement guidelines for creating safe environments for the trans community in Canada such as the ‘Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People’ - provided by the WPATH.
Conduct research in partnership with diverse groups of transgender individuals to design, implement, and evaluate transgender-specific health care programs and services.
Include questions and information about gender identity on national surveys and health-related data sets.
Trans people in Ontario span a range of ages and occupations, and are geographically and proportionally distributed across the province- a report by Trans PULSE stated. About one in five trans people do not identify as male or female, or even as primarily masculine or feminine. These more gender-fluid people can identify as both male and female, neither male nor female, or as something else entirely.
Ahmad said research shows by the time a trans-individual is engaging you for hormonal care, they are often at their most vulnerable and at higher risk for suicide.
She said gender-affirming procedures are not cosmetic but necessary.
"They are truly lifesaving," Ahmad said. "Trans care is health care, trans rights are human rights, and gender-affirming care is life-saving.”






Comments